Breast reduction surgery provides multiple advantages yet comes with inherent risks. Gaining insight into both the surgical steps involved and the possible side effects allows people to make well-informed choices and get properly ready for the operation.
Female-to-male chest reduction surgery, often referred to as a gender-confirming chest reconstruction mastectomy, is akin to an inverted-T mastopexy procedure. During this operation, the surgeon removes breast tissue, glands, and surplus skin.
Nonetheless, similar to all surgical procedures, this one also involves possible risks, including hemorrhaging, seroma development, infections, tissue death, altered sensations or extended numbness, and excessive scarring. Here are some perspectives provided by Dr. Ho Cao Vu concerning typical issues linked with female-to-male breast reduction surgeries.
Hematoma
A hematoma may develop soon following breast reduction surgery, frequently as a result of insufficient clotting control during the operation. Should the bleeding be slight, the body has the ability to absorb the blood internally without intervention. Nonetheless, substantial hemorrhaging might cause the development of a hematoma.
The breast comprises skin, adipose tissue, glandular tissue, and supportive connective tissues known as stromal tissue. Embedded within this stroma is an intricate system of blood vessels and lymphatic channels. Primary arterial supplies come from the lateral thoracic artery along with the anterior and posterior intercostal perforators. These branches create a vascular web within the front fatty section, which can lead to increased risk of significant bleeding during breast reduction operations when contrasted with typical breast enlargement surgeries.
A hematoma appears as swelling, pain, and bruising, which may restrict blood circulation. This increases the chances of infection and extended inflammation. Such issues can jeopardize the health of the skin flap, hinder recovery, and possibly lead to irregularities in the breast shape.
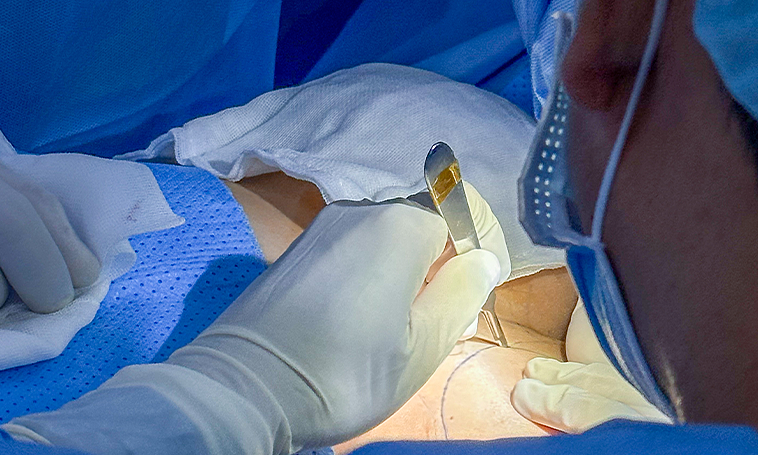
|
|
Female-to-male chest reduction surgery comes with risks that should be thoroughly considered. Photo courtesy of Dung Ho |
Infection
One of the initial complications after female-to-male chest masculinizing surgery can be an infection. This usually appears as localized swelling and redness and is commonly treated with oral antibiotics. Nevertheless, should the infection continue unabated even when medicated, procedures such as surgical draining or removal of damaged tissue might become necessary.
The majority of post-surgical infections typically arise from the third to the seventh day following the operation; however, certain cases might manifest subsequently. Indications of an infection comprise diminished hunger, changes in flavor perception, elevated body temperature, discomfort around the incision area, redness, or puffiness.
{getCard} $type={post} $title={You might like}
Dr. Vu suggests that if any of these symptoms appear, an early assessment by a surgeon should be sought. Should the infection not respond to antibiotic treatment, surgery might be required to cleanse the affected region, remove infected tissue, and eliminate built-up fluids.
Nipple-areola necrosis
Tissue death of the nipple-areola area can occur as a result of reduced blood flow, frequently because of significant harm to the surrounding tissues induced by surgery or burning treatments like cauterization.
Loss of sensation
Numbness in the breast and nipples is frequently experienced after surgical procedures that involve cuts near the nipple-areola area.
People with smaller breasts and less glandular tissue might minimize the chance of losing sensation by choosing preservation-focused surgical methods and precisely locating cuts during the procedure.
For individuals with substantial glandular tissue or aged skin, the likelihood of encountering complications increases. Employing electrocautery for tissue removal at elevated temperatures might result in thermal injury, which could lead to decreased sensitivity, numbness, or even total loss of feeling in the nipple area.
Unfavorable scarring
The appearance of scars relies heavily on the surgeon’s technique and their ability to evaluate skin elasticity along with the potential for scar development. A meticulously planned surgical strategy, alongside adequate pre-, intra-, and post-operative scar treatment, can significantly reduce the likelihood of developing thickened or constrictive scars. Scar formation is an unavoidable aspect of breast reduction surgeries; however, its extent hinges upon both the chosen surgical procedure and how diligently one follows post-surgical care instructions.
Comprehensive preoperative tests are essential for breast reduction surgery to exclude issues like clotting disorders and high blood pressure, along with stopping the use of anticoagulant drugs and specific herbal remedies. Although uncommon, anesthesia poses potential hazards such as airway blockage, heart rhythm abnormalities, allergic responses, brain damage, strokes, and in severe cases, fatalities.
To reduce surgical risks, it is advised to have breast reduction procedures performed at accredited hospitals, ideally those with multiple specialties, that hold approval from the Ministry of Health. This ensures both your safety and immediate access to medical care should any issues develop during or after the surgery.

|
|
Scarring is an unavoidable part of breast reduction surgery, with its extent varying based on the chosen surgical approach, techniques employed, and aftercare following the procedure. Photo courtesy Dung Ho |
Benefits of Employing an Ultrasonic Scalpel
Dr. Vu emphasizes the advantages of the advanced Ultrasonic Surgical Scalpel, equipped with an embedded chip for managing coagulation, sealing, and cutting functionalities. This innovation improves surgical safety, particularly during breast reduction surgeries where substantial portions of glandular tissue and skin must be removed.
The ultrasonic scalpel provides numerous benefits after surgery, such as reducing pain by up to 90%, allowing patients to be discharged on the same day, eliminating the requirement for extra pain medication, promoting quicker and smoother healing of scars more effectively than electrocautery, and decreasing both immediate and long-term complications. This tool employs high-frequency sound waves to cut through tissues with precision, limiting harm to nearby healthy areas, thereby accelerating recovery and lessening discomfort, notably during procedures like female-to-male chest masculinization and breast lift operations for drooping chests.

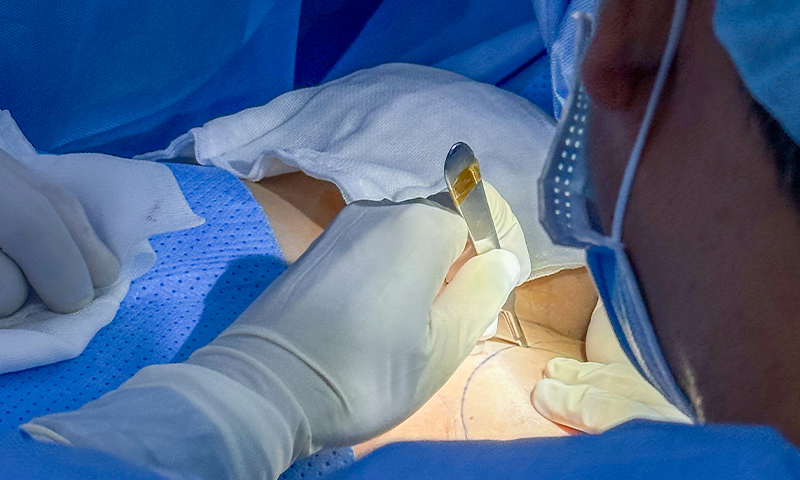
|
|
The advanced Ultrasonic Surgical Scalpel improves surgical safety, especially during breast reduction surgeries that involve removing substantial amounts of glandular tissue and additional skin. Image provided by Dung Ho |
Surgical procedure
The process starts with evaluating the present state of the breasts, covering glandular tissue, soft tissue, any unusual lumps, skin composition, and the framework of the ribs. The doctor will outline where to make an incision and create a strategy for safely removing tissue. Repositioning the nipple-areola complex might be necessary, particularly when dealing with drooping breasts or notable downward displacement of the glandular area past the lower part of the breast, alongside overly loose skin. Efforts are made to prevent taking out too much glandular and soft tissue as this can disrupt blood flow, raising chances of issues like dead wounds, lack of oxygen supply to the nipple-areola region, and thickened scars.
In the subsequent phase of tissue dissection and liberation, simultaneous hemostasis and blood management are achieved via coagulation and sealing techniques, which significantly reduce postoperative serous fluid buildup while maintaining precise surgery standards. The use of an ultrasonic scalpel during this process helps minimize thermal damage, expedite recovery times, and lower risks such as serous effusions and excessive scar tissue death associated with hypertrophy.
The last step includes stitching to facilitate quick recovery and achieve the best possible cosmetic outcome.
